Inserted into a tracheostoma, the tracheostomy tube ensures access to the lower respiratory tract when breathing is no longer possible naturally. It offers those affected significantly more comfort and a more independent life than a breathing tube through the mouth.
After appropriate training, tracheostomy tubes can largely be cleaned and supplied by yourself. This article explains when a tracheostomy tube is necessary and how to put it on.
What is a tracheostomy tube?
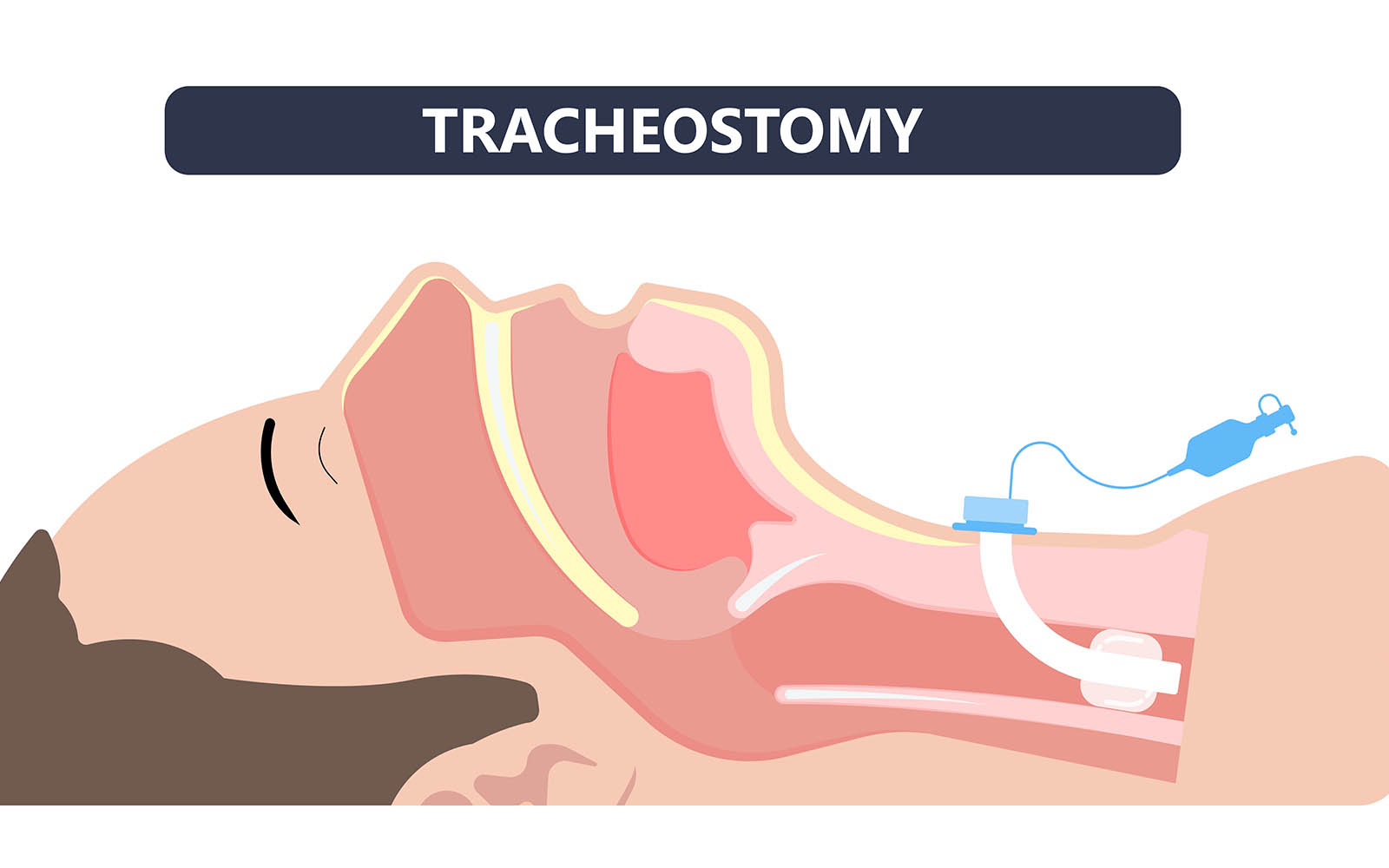
A tracheostomy tube is a tube that connects the windpipe directly to the outside air, bypassing the natural airway. The insertion of the tracheostomy tube is usually carried out as part of a tracheostomy (tracheotomy), especially in long-term ventilators. The hole created in the trachea, the tracheostoma, forms the channel through which the tracheostomy tube is inserted.
field of use
Various diseases of the upper respiratory tract may require the use of a tracheostomy tube.
Cancers of the throat or in the larynx area often lead to a massive narrowing of the airways due to displacing growth. Bleeding, mucus and swelling caused by the accompanying inflammation are just as problematic as tissue damage caused by local radiation.
Nerve damage caused by accidental injuries, a stroke or chronic illnesses can lead to the muscles in the respiratory tract no longer being controlled properly. Thyroid diseases or operations also pose a high risk of breathing problems. This is because fine muscle movements have to open the vocal cords for breathing and voice production and the associated nerve branches run directly in the thyroid tissue. An interruption in nerve impulses causes the airways to no longer open. An emergency tracheostomy is then necessary so that those affected can breathe.
Tracheostomy tubes can be used in long-term ventilation in the intensive care unit as well as in nursing homes and in intensive home care. It offers many advantages over ventilation via the mouth. The artificial airways are significantly shorter after a tracheostomy, so that the airway resistance is lower and ventilation is more gentle. In addition, those affected are significantly less restricted and the tracheostomy tube is not immediately noticeable. This means a better quality of life.
Tracheostomy tube – structure and types
A tracheostomy tube is a slightly curved tube that can be held in place with a holder that sits like a bow tie in front of the neck. Depending on the treatment goal and the condition of the surrounding tissue, the cannula is made of different materials, such as silicone or polyurethane, but also plastic or silver.
There are cannulas of different lengths and curvatures. They are available with or without a cuff and consist of just one or two tubes one inside the other.
A speaking valve can be installed in patients who still have an intact larynx. When you exhale, this does not direct the air back out through the cannula, but through the larynx, which enables speaking with intact muscles and nerves . If the larynx is removed, other methods must be used to restore speech.
With or without blocking?
Whether or not a cuff block is required depends on the patient’s condition. If there is a high risk of choking or if there is no urge to cough, the airways must be securely sealed at the top. If those affected then want to speak with a speaking valve, the cuff must be unblocked for a short time so that they can breathe out the air through the larynx.
Attach tracheostomy tube
To create a tracheostomy tube, you first perform a tracheostomy, i.e. creating an opening in the trachea. This can be done through a surgical procedure in which a small soft tissue window is cut into the trachea and associated cartilage. The opening is lined with skin from the surface of the neck, which is folded inward and sutured directly to the trachea. The surgeon then inserts the first tracheostomy tube and fixes the holding plate.
Alternatively, a tracheostomy can also work via percutaneous dilatation. With this technique, the doctor uses a hollow needle to pierce the skin into the trachea and then widens the hole using dilators until the cannula can be pushed in.
When to change the tracheostomy tube?
A tracheostomy tube should always be changed when necessary and at the latest after a fixed rhythm. In systems with two tubes lying one inside the other, the inner tube is usually changed after a few days to a few weeks. The outside is usually replaced at monthly intervals. However, the inner cannula must be cleaned much more frequently, usually twice or three times a day, or more often in acute illnesses.
Tracheostomy tube – supply and care
The tracheostomy tube is often the vital safeguard of the airway and must be cared for appropriately because complications can have acute, life-threatening consequences.
Care at home
After appropriate training and initial support from a nursing service, caring for a tracheostomy with an inserted cannula is usually also possible for people who are not medically trained. The tracheostoma should be cleaned twice a day with washed hands. Then you change the compress that is attached to the skin. This can also involve suctioning out mucus and inspecting the skin.
The system usually consists of two cannulas, an inner and an outer one. Those affected can also rinse the inner one daily and change it as needed. The outer cannula is usually changed by a doctor or an appropriately trained nursing staff member.
Tracheostomy tube – Possible complications
Complications of a lying tracheostomy tube affect, on the one hand, the skin in the area of the cannula and, on the other hand, the access itself. Pressure ulcers at the fixation and local irritations can be detected early through close observation and severe forms can be prevented.
Lesions within the trachea caused by an overly blocked cuff are more difficult to detect, so regular pressure measurement is essential. Infections can be avoided through good hygiene and regular cannula changes. If patients produce a lot of secretion such as mucus or blood in the airways, this can block the cannula.
There is always a risk of the cannula slipping, especially with mobile patients. Good and secure fixation reduces the risk of the cannula becoming loose. When changing the outer cannula, one must always expect a possible collapse of the tracheostoma, which would acutely close the artificial airway. In this case, an oxygen tube can be inserted as an emergency and the opening can be restored in various ways.
- : public

